
Lupus is an autoimmune condition that causes the immune system to attack healthy tissues. While traditional treatments like immunosuppressants and anti-inflammatory drugs provide some relief, they often fall short of addressing the root causes of lupus. Stem cell therapy, an emerging treatment, offers a revolutionary approach by targeting the disease at its core.
Here are the top four benefits of stem cell therapy for lupus patients.
Table of Contents
3 Key Considerations Before Choosing Stem Cell Therapy for Lupus
Top 4 Benefits of Stem Cell Therapy for Lupus Patients
Benefit 1: Regenerating Damaged Tissues
Benefit 2: Reducing Chronic Inflammation
Benefit 3: Modulating Immune System Responses
Benefit 4: Enhancing Overall Quality of Life
How to Choose the Right Healthcare Provider for Stem Cell Therapy
What to Expect From Stem Cell Therapy for Lupus
Take the Leap Toward Better Lupus Care with BioRestore!
| Key Takeaways ✔ Stem cell therapy repairs damaged organs such as the kidneys, lungs, and heart by promoting tissue regeneration and improving their functionality, reducing the risk of severe complications. ✔ Stem cells release anti-inflammatory proteins that lower swelling, pain, and stiffness, providing immediate relief and preventing long-term tissue damage. ✔ Stem cell therapy rebalances immune responses, reducing autoimmune activity while preserving the body’s ability to fight infections and minimizing lupus flares. ✔ By increasing energy levels, improving mobility, and supporting mental health, stem cell therapy helps patients regain independence and achieve a better overall quality of life. |
What Is Lupus?
Lupus is a chronic autoimmune disease that causes the immune system to attack healthy tissues and organs. This abnormal immune response leads to widespread inflammation and can impact multiple systems in the body.
It is estimated that over 200,000 people in the United States are living with lupus. The condition is unpredictable, with periods of remission followed by flare-ups that exacerbate symptoms. Though lupus can affect anyone, it is more commonly diagnosed in women, particularly those of childbearing age, and tends to be more severe in individuals of African, Hispanic, or Asian descent.
Common Symptoms of Lupus
Lupus manifests differently in each patient, but some symptoms are more prevalent and can significantly impair a person’s quality of life. These include:
- Chronic Fatigue: Persistent exhaustion is one of the most reported symptoms. Unlike ordinary tiredness, this fatigue often does not improve with rest and can interfere with work, family life, and hobbies.
- Joint Pain and Stiffness: Inflammation in the joints, known as lupus arthritis, can cause swelling, pain, and reduced mobility. This is particularly challenging for patients who need to remain active for daily activities.
- Organ Damage: Lupus can harm vital organs over time, including:
- Kidneys: Lupus nephritis, a serious complication, can impair kidney function and lead to renal failure.
- Heart: Inflammation can increase the risk of cardiovascular disease, one of the leading causes of death in lupus patients.
- Lungs: Scarring and inflammation in the lungs can cause shortness of breath and chronic respiratory issues.
- Skin Issues: Many patients experience rashes, particularly the “butterfly rash” that spreads across the nose and cheeks. Photosensitivity is also common, with exposure to sunlight triggering or worsening skin lesions.
- Cognitive Issues: Some individuals report memory problems, confusion, and difficulty concentrating, often referred to as “lupus fog.”
Challenges With Current Treatments
Traditional treatments for lupus aim to suppress the immune system or control inflammation. Common approaches include:
- Corticosteroids: These medications reduce inflammation quickly but come with side effects such as weight gain, increased risk of infections, and bone thinning with prolonged use.
- Immunosuppressants: Drugs like methotrexate and cyclophosphamide help control immune system activity but can leave patients more susceptible to infections.
- Antimalarials: Medications like hydroxychloroquine are used to manage skin and joint symptoms but may take months to show effects.
3 Key Considerations Before Choosing Stem Cell Therapy for Lupus
There is a growing interest in stem cell therapy, as the market is expected to grow at a compound annual growth rate (CAGR) of 25.23% between 2025 and 2030. However, while the potential for symptom relief and improved quality of life is significant, it is essential to consider several factors before pursuing stem cell therapy, including risks, eligibility, and preparation requirements.
1. Assess Eligibility for Stem Cell Therapy
- Evaluate Condition: Determining the ideal candidate must be based on disease severity, current treatment responses, and overall health.
- Address Existing Health Issues: Resolve any active infections or severe health conditions before starting therapy.
- Consult a Specialist: Seek advice from a qualified healthcare provider to confirm suitability for stem cell therapy.
2. Understand Potential Risks and Side Effects
- Recognize Common Risks: Be aware of possible complications such as infection, blood clots, or immune reactions with donor stem cells.
- Consider Rare Complications: Discuss risks like tumor formation or adverse immune responses with the provider.
- Minimize Risks Through Screening: Ensure proper screening and the use of high-quality, processed stem cells to reduce potential issues.
3. Evaluate Costs and Financial Considerations
- Check Insurance Coverage: Confirm whether insurance covers stem cell therapy, as it is often deemed experimental.
- Understand Total Costs: Assess expenses for consultations, cell harvesting, follow-ups, and additional services.
- Explore Financial Options: Look into financing plans or alternative payment methods if insurance does not cover the treatment.
Top 4 Benefits of Stem Cell Therapy for Lupus Patients
Benefit 1: Regenerating Damaged Tissues
One of the most remarkable aspects of stem cell therapy is its ability to repair damaged tissues. Over time, lupus can cause extensive damage to vital organs, including:
- Kidneys: Lupus nephritis, a common complication, can impair kidney function and lead to renal failure. Left untreated, this condition can progress rapidly and require dialysis or even a kidney transplant to sustain life.
- Lungs: Chronic inflammation may result in lung scarring and reduced respiratory capacity. This can lead to complications like chronic cough, shortness of breath, and an increased susceptibility to respiratory infections.
- Heart: Lupus patients are at a higher risk of cardiovascular issues due to ongoing tissue damage. This can contribute to conditions such as pericarditis, heart attacks, and arrhythmias, which further complicates the management of lupus.
How Stem Cell Therapy Helps
- Stimulating Natural Healing Processes: Stem cells release growth factors that stimulate the body’s natural healing processes, initiating tissue repair where it is needed most. These growth factors promote cell regeneration and blood vessel formation, which ensures a steady supply of nutrients and oxygen to damaged areas.
- Replacing Damaged or Scarred Cells: These cells can differentiate into tissue-specific types and replace damaged or scarred cells with healthy, functional ones. For example, stem cells can transform into kidney cells to repair lupus nephritis or lung cells to reverse scarring.
- Improving Organ Function and Preventing Complications: The regenerative properties of stem cells prevent further complications that may arise from chronic damage. By restoring optimal functionality to critical organs such as the heart, kidneys, and lungs, stem cell therapy reduces the risk of life-threatening conditions,
Benefit 2: Reducing Chronic Inflammation
Chronic inflammation is one of the primary drivers of lupus symptoms. It contributes to:
- Joint Pain and Swelling: Affects mobility and causes significant discomfort. Over time, untreated inflammation in the joints can lead to deformities, loss of joint function, and chronic stiffness, making everyday tasks increasingly challenging.
- Skin Issues: Prolonged inflammation exacerbates rashes and sensitivity. Severe cases can lead to scarring and discoloration, which may affect a patient’s confidence and contribute to emotional distress.
- Systemic Fatigue: Chronic inflammation places a constant strain on the body, contributing to extreme fatigue that does not improve with rest. This reduces energy levels and impacts the ability to engage in daily activities.
How Stem Cell Therapy Reduces Inflammation
- Suppressing Inflammatory Responses: Stem cells release anti-inflammatory cytokines, proteins that suppress the body’s inflammatory response. These cytokines work to regulate the overactive immune system, calming the chronic inflammation that is a hallmark of lupus.
- Reducing Swelling, Pain, and Stiffness: By targeting inflammation at the cellular level, stem cell therapy reduces swelling, pain, and stiffness. This allows patients to regain mobility and perform daily activities more comfortably, improving their overall well-being.
- Stabilizing the Condition and Reducing Flares: This effect also lowers the frequency and severity of lupus flares, offering patients more stability in their condition. Over time, the consistent reduction in inflammation helps prevent further tissue damage and slows disease progression.
Benefit 3: Modulating Immune System Responses
Lupus is fundamentally an autoimmune disorder, meaning the immune system mistakenly attacks the body’s healthy tissues. This misfire leads to the widespread symptoms and complications lupus patients face.
How Stem Cell Therapy Modulates the Immune System
- Regulating Immune Responses: Stem cells work to regulate immune responses, preventing overactive immune cells from targeting healthy tissues. By interacting with key immune components, such as T-cells and B-cells, stem cells reduce the autoimmune attack that causes lupus symptoms.
- Reducing Autoimmune Activity While Preserving Defense: By restoring immune balance, stem cell therapy reduces autoimmune activity without compromising the body’s ability to fight infections. Unlike traditional immunosuppressants that weaken the entire immune system, stem cell therapy takes a more selective approach, ensuring that patients remain protected against everyday illnesses and infections.
- Strengthening Immune System Resilience: Stem cell therapy not only calms overactive immune responses but also promotes long-term immune system stability. This reduces the risk of additional autoimmune complications and helps patients maintain overall immune health.
Benefit 4: Enhancing Overall Quality of Life
Living with lupus takes a toll on both physical and emotional well-being. Symptoms like fatigue, pain, and organ dysfunction can make even basic tasks challenging. Stem cell therapy addresses these issues holistically, leading to significant improvements in patients’ daily lives.
How Stem Cell Therapy Improves Quality of Life
- Increased Energy Levels: By reducing inflammation and promoting healing, patients often feel more energized. This newfound energy helps them regain the stamina needed to engage in daily activities, work, and hobbies that were previously hindered by fatigue.
- Improved Mobility: Relief from joint pain and swelling allows for greater physical activity. Enhanced mobility not only boosts physical health but also promotes independence, enabling patients to participate more fully in social and recreational activities.
- Mental Health Benefits: Managing symptoms effectively can reduce stress, anxiety, and depression associated with lupus. This positive shift in mental well-being fosters a greater sense of control over the disease and improves overall emotional resilience.
How to Choose the Right Healthcare Provider for Stem Cell Therapy
Choosing the right provider in Connecticut ensures a safe and effective treatment experience, allowing lupus patients to gain the full benefits of stem cell therapy. By following these steps, patients can make informed and confident decisions about their care:
1. Verify Credentials and Expertise
Confirm the provider has extensive experience with stem cell therapy, particularly for autoimmune conditions like lupus. Check for certifications and affiliations with reputable medical organizations to ensure high standards of care.
2. Research Reputation and Success Stories
Look for patient reviews and case studies to evaluate the provider’s track record. Seek positive feedback from lupus patients to gain insights into the clinic’s quality of care and treatment outcomes involving stem cell therapy.
3. Demand Personalized Treatment Plans
Ensure the provider develops customized treatment plans based on the individual’s unique medical history and condition. Confirm that the plan includes ongoing monitoring and adjustments to maximize the therapy’s effectiveness.
4. Require Transparency and Communication
Insist that the provider clearly explains the treatment process, potential risks, and expected outcomes. Encourage open discussions where patients can freely ask questions and receive honest answers.
5. Confirm the Use of Cutting-Edge Technology
Verify that the clinic utilizes advanced equipment and techniques for harvesting, processing, and administering stem cell therapy. Ensure that modern technology is in place to minimize risks and optimize results.
6. Prioritize Patient Safety
Check that the provider adheres to strict safety protocols, including sterile procedures and regulatory compliance. Ensure a thorough pre-treatment evaluation is conducted to identify risks and contraindications for the therapy.
What to Expect From Stem Cell Therapy for Lupus
Understanding the treatment process helps patients prepare for what lies ahead. Results vary, but many lupus patients experience significant relief from symptoms and improved overall health after undergoing stem cell therapy. Here’s what lupus patients can expect:
- Initial Consultation: The healthcare provider evaluates the patient’s medical history, current symptoms, and treatment goals. This determines if stem cell therapy is suitable for the individual.
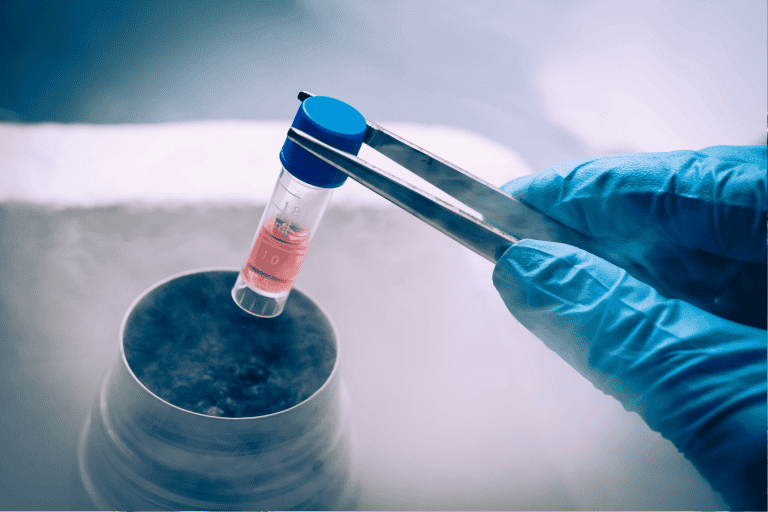
- Stem Cell Harvesting and Preparation: Stem cells are typically harvested from the patient’s own bone marrow or adipose tissue. These cells are then processed to ensure they are viable and ready for therapeutic use.
- Treatment Administration: Stem cells are delivered through intravenous infusion or targeted injections, depending on the treatment plan. The procedure is minimally invasive and often requires little to no downtime.
- Recovery and Follow-Up: Patients may notice gradual improvements over weeks or months. Regular follow-ups with the healthcare provider monitor progress and address any concerns.
Frequently Asked Questions
What are the potential risks and side effects of stem cell therapy for lupus?
Stem cell therapy, while promising, carries some risks that should be carefully considered. Potential side effects include infection, immune rejection, or graft-versus-host disease in cases where donor cells are used. Rarely, there may also be a risk of abnormal cell growth leading to malignancies. It is essential to consult a qualified healthcare provider to understand and minimize these risks before undergoing treatment.
How long does it take to see results from stem cell therapy in lupus patients?
The timeline for seeing results from stem cell therapy varies from patient to patient. Some individuals notice improvements in symptoms such as reduced inflammation and pain within a few weeks, while others may take several months to experience significant changes. Consistent follow-up care and monitoring are critical to evaluate the therapy’s effectiveness and address any concerns during the recovery process.
Is stem cell therapy for lupus covered by insurance?
Insurance coverage for stem cell therapy often depends on the provider and the specific type of treatment. Many insurance companies consider stem cell therapy to be experimental and may not cover the costs. Patients should speak with their insurance representatives to confirm their coverage and explore alternative funding options if necessary.
What is the success rate of stem cell therapy in treating lupus?
The success rate of stem cell therapy for lupus depends on various factors, including the severity of the condition, the patient’s overall health, and the type of stem cells used. Clinical studies have shown promising results, with many patients reporting reduced disease activity and fewer flares. However, more research is needed to establish long-term success rates and outcomes.
Are there any clinical trials for stem cell therapy in lupus patients?
Yes, numerous clinical trials are currently investigating the safety and efficacy of stem cell therapy for lupus. These studies aim to refine treatment protocols and better understand how stem cells can improve outcomes for lupus patients. Those interested in participating should consult their healthcare providers or visit clinical trial databases to find opportunities tailored to their needs

Take the Leap Toward Better Lupus Care with BioRestore!
If you’re ready to explore how stem cell therapy can transform your lupus management, turn to BioRestore for expert care. As a trusted provider based in Connecticut, BioRestore offers cutting-edge treatments tailored to your unique needs. With our state-of-the-art facility and a team dedicated to patient success, we are committed to helping you achieve a better quality of life.
Contact BioRestore in Connecticut today to schedule a consultation and discover how this advanced treatment can help you regain control over your lupus symptoms!